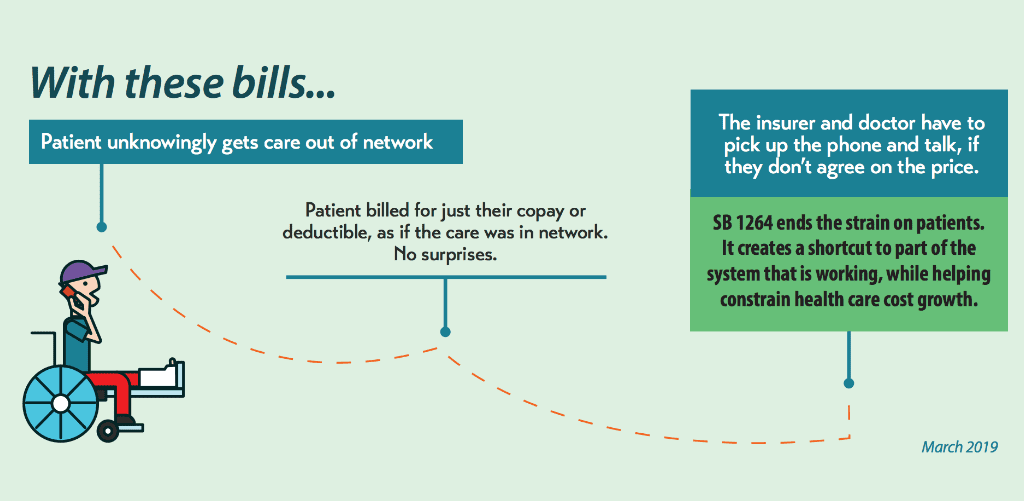
Surprise medical bills are a big problem for Texans, as shown by numerous recent media stories. Fortunately, the 2019 Texas Legislature is working to remove patients from fights between insurers and health care providers over prices and to end surprise, out-of-network bills. We are excited that the Senate has passed Chairman Kelly Hancock’s Senate Bill 1264 by a wide margin.
Surprise medical bills happen when insurers and doctors or other health care providers – fighting over prices – jointly pass the buck to a patient, who received out-of-network health care unknowingly. Surprise billing is especially common in an emergency – when sick or injured patients must rush to the nearest emergency room and have no ability to choose the doctors who treat them.

However, one narrow issue within that larger debate of how to end surprise billing is how to best identify which out-of-network bills are truly “surprises.” This means figuring out when the charges stem from health care services where the patient had no choice in their health care providers and unknowingly received care out of their network.
Good proposals at the Legislature from State Rep. John Smithee (R-Amarillo) and State Sen. Nathan Johnson (D-Dallas) – House Bill 1742 and Senate Bill 1914 – close an inadvertent loophole in our current system and also help identify another source of surprise medical bills.
The Texas Legislature has taken steps over the last decade to build and improve a dispute resolution system for surprise medical bills – specifically to help those consumers who, despite taking all of the right steps, had no ability to avoid a surprise out-of-network medical bill.
Last session, the Texas Legislature passed Senate Bill 507 by Chairman Hancock, which tried to identify all of the possible scenarios where a consumer could unknowingly get out-of-network health care, and wrap them into the state’s surprise billing mediation system.
Shortly after that bill took effect, Kaiser Health News and NPR released a feature story about a woman in Houston. She got a $17,850 surprise, out-of-network medical bill from a lab following a urine test at her in-network doctor’s office. She could not turn to mediation because surprise bills from labs are not eligible under current Texas law, even though patients get no choice in which lab a specimen is sent to. This egregious example, with an astronomically high out-of-network lab bill, demonstrates the need for additional patient protections.
This is another example where the patient did the right thing – she was at an in-network doctor’s office. Yet, the patient had no choice in lab provider, and may not have even known that the specimen was being sent to an off-site lab for processing, so she had no ability to avoid the surprise medical bill.
Rep. Smithee’s HB 1742 and Sen. Johnson’s SB 1914 add out-of-network labs to the existing mediation system if a patient has a specimen collected at an in-network doctor’s office or hospital and it is then sent to an out-of-network lab without their knowledge.
These companion bills build on work from
CPPP Health & Wellness Intern Kevin P. Caudill wrote this piece.